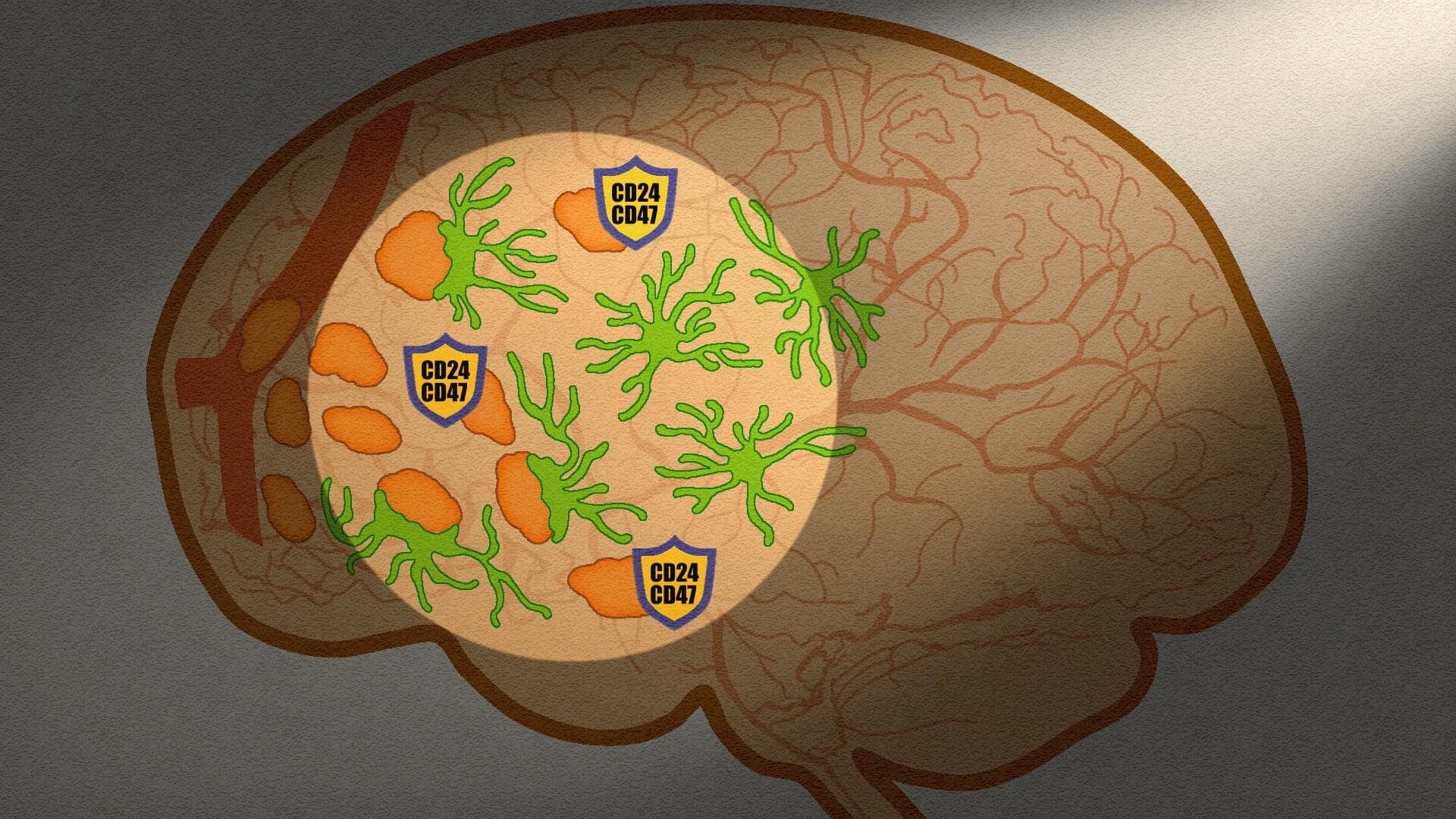
For the first time, a team of researchers at the Institute for Neurosciences (IN), a joint center of the Spanish National Research Council (CSIC) and Miguel Hernández University of Elche (UMH), has reconstructed how the cerebellum establishes its connections with the rest of the brain during the earliest stages of life.
The work, published in the journal Proceedings of the National Academy of Sciences, describes in detail the phases during which these neural connections emerge, expand, and are refined, offering the first comprehensive map of the development of cerebellar projections across the mouse brain.
Although the cerebellum has traditionally been associated with motor control, growing evidence shows that it also plays a role in processes such as emotional regulation, social behavior, and other cognitive functions. However, until now, it was not precisely known when it began interacting with other regions of the brain, communication that is fundamental for these cerebellar roles. This gap motivated the work of the group Development, Wiring and Function of Cerebellar Circuits, led by Juan Antonio Moreno Bravo at the IN.